Staphylococcus epidermidis: Diferenzas entre revisións
traducido de en:Staphylococcus epidermidis |
(Sen diferenzas.)
|
Revisión como estaba o 21 de marzo de 2014 ás 10:13
Este artigo está a ser traducido ao galego por un usuario desta Wikipedia; por favor, non o edite. O usuario Miguelferig (conversa · contribucións) realizou a última edición na páxina hai 10 anos. Se o usuario non publica a tradución nun prazo de trinta días, procederase ó seu borrado rápido. |
| Staphylococcus epidermidis | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 Scanning electron image of S. epidermidis. | |||||||||||||||
| Clasificación científica | |||||||||||||||
| |||||||||||||||
| Nome binomial | |||||||||||||||
| 'Staphylococcus epidermidis' (Winslow & Winslow 1908) Evans 1916 | |||||||||||||||
| Sinonimia | |||||||||||||||
|
Staphylococcus albus Rosenbach 1884 | |||||||||||||||
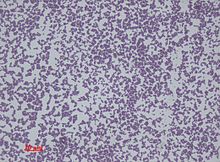
Staphylococcus epidermidis é unha especie bacteriana Gram positiva, unha das arredor de 40 especies pertencentes ao xénero Staphylococcus.[1] Forma parte da flora bacteriana humana normal, normalmente da flora da pel, e máis raramente da flora das mucosas.[2] Aínda que S. epidermidis xeralmente non é patoxénica, as persoas con sistemas inmunitarios inmunocomprometidos están en risco de desenvolver a infección. Estas infeccións adquírense xeralmente en hospitais (infeccións nosocomiais).[3] S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices.[4] Being part of the normal skin flora, S. epidermidis is a frequent contaminant of specimens sent to the diagnostic laboratory.[5]
Descubrimento
Esta especie foi distinguida por Friedrich Julius Rosenbach de Staphylococcus aureus en 1884, e inicialmente deulle o nome de S. albus.[6] Elixiu os nomes aureus e albus para estas dúas especies porque formaban, respectivamente, colonias de cor amarela e branca. Posteriormente o nome cambiouse a epidermidis.
Morfoloxía celular e bioquímica
S. epidermidis is a very hardy microorganism, consisting of nonmotile, Gram-positive cocci, arranged in grape-like clusters. It forms white, raised, cohesive colonies approximately 1–2 millimeter in diameter after overnight incubation, and is nonhemolytic on blood agar.[4] But the regular size/diameter of S. epidermis is approximately 0.5 to 1.5 micrometers. It is a catalase-positive,[7] coagulase-negative, facultative anaerobe that can grow by aerobic respiration or by fermentation. Some strains may not ferment.[8]
Biochemical tests indicate this microorganism also carries out a weakly positive reaction to the nitrate reductase test. It is positive for urease production, is oxidase negative, and can use glucose, sucrose, and lactose to form acid products. In the presence of lactose, it will also produce gas. S. epidermidis does not possess the gelatinase enzyme, so it cannot hydrolyze gelatin.[Cómpre referencia] It is sensitive to novobiocin, providing an important test to distinguish it from Staphylococcus saprophyticus, which is coagulase-negative, as well, but novobiocin-resistant.[3]
Similar to those of Staphylococcus aureus, the cell walls of S. epidermidis have a transferrin binding protein that helps the organism obtain iron from transferrin. The tetramers of a surface exposed protein, glyceraldehyde-3-phosphate dehydrogenase, are believed to bind to transferrin and remove its iron. Subsequent steps include iron being transferred to surface lipoproteins, then to transport proteins which carry the iron into the cell.[4]
Virulencia e resistencia a antibióticos
The ability to form biofilms on plastic devices is a major virulence factor for S. epidermidis. One probable cause is surface proteins that bind blood and extracellular matrix proteins. Staphylococcus epidermidis produces an extracellular polysaccharide material known as polysaccharide intercellular adhesion (PIA), which is made up of sulfated polysaccharide. It allows other bacteria to bind to the already existing biofilm, creating a multilayer biofilm. Such biofilms decrease the metabolic activity of bacteria within them. This decreased metabolism, in combination with impaired diffusion of antibiotics, makes it difficult for antibiotics to effectively clear this type of infection.[4] S. epidermidis strains are often resistant to antibiotics, including penicillin, amoxicillin, and methicillin. Resistant organisms are most commonly found in the intestine, but organisms living freely on the skin can also become resistant due to routine exposure to antibiotics secreted in sweat.
Enfermidades
As mentioned above, S. epidermidis causes biofilms to grow on plastic devices placed within the body.[9] This occurs most commonly on intravenous catheters and on medical prostheses.[10] Infection can also occur in dialysis patients or anyone with an implanted plastic device that may have been contaminated. Another disease it causes is endocarditis. This occurs most often in patients with defective heart valves. In some other cases, sepsis can occur in hospital patients. [Cómpre referencia]
Antibiotics are largely ineffective in clearing biofilms. The most common treatment for these infections is to remove or replace the infected implant, though in all cases, prevention is ideal. The drug of choice is often vancomycin, to which rifampin or aminoglycoside can be added.[Cómpre referencia] Hand washing has been shown to reduce the spread of infection.
Preliminary research also indicates S. epidermidis is universally found inside affected acne vulgaris pores, where Propionibacterium acnes is normally the sole resident.[11]
Identificación
The normal practice of detecting S. epidermidis is by using the Baird-Parker agar with egg yolk supplement. Colonies appear small and black. They can be confirmed using the coagulase test. Increasingly, techniques such as quantitative PCR are being employed for the rapid detection and identification of Staphylococcus strains.[12][13] Normally, sensitivity to desferrioxamine can also be used to distinguish it from most other staphylococci, except in the case of Staphylococcus hominis, which is also sensitive. In this case, the production of acid from trehalose by S. hominis can be used to tell the two species apart.
Notas
- ↑ Schleifer, K. H.; Kloos, W. E. (1975). "Isolation and Characterization of Staphylococci from Human Skin I. Amended Descriptions of Staphylococcus epidermidis and Staphylococcus saprophyticus and Descriptions of Three New Species: Staphylococcus cohnii, Staphylococcus haemolyticus, and Staphylococcus xylosus". International Journal of Systematic Bacteriology 25 (1): 50–61. ISSN 0020-7713. doi:10.1099/00207713-25-1-50.
- ↑ Fey, P. D.; Olson, M. E. (2010). "Current concepts in biofilm formation of Staphylococcus epidermidis". Future Microbiology 5 (6): 917–933. doi:10.2217/fmb.10.56.
- ↑ 3,0 3,1 Levinson, W. (2010). Review of Medical Microbiology and Immunology (11th ed.). pp. 94–99.
- ↑ 4,0 4,1 4,2 4,3 Salyers, Abigail A. and Whitt, Dixie D. (2002). Bacterial Pathogenesis: A Molecular Approach, 2nd ed. Washington, D.C.: ASM Press. ISBN 1-55581-171-X.
- ↑ Queck SY and Otto M (2008). "Staphylococcus epidermidis and other Coagulase-Negative Staphylococci". Staphylococcus: Molecular Genetics. Caister Academic Press. ISBN 978-1-904455-29-5.
- ↑ Friedrich Julius Rosenbach en Who Named It?
- ↑ "Todar's Online Textbook of Bacteriology: Staphylococcus aureus and Staphylococcal Disease". Kenneth Todar, PhD. Consultado o Dec 7, 2013.
- ↑ "Bacteria Genomes - STAPHYLOCOCCUS EPIDERMIDIS". Karyn's Genomes. EMBL-EBI. Consultado o December 23, 2011.
- ↑ Modelo desbotado. Use un dos modelos de citas no lugar deste marcador.
- ↑ Modelo desbotado. Use un dos modelos de citas no lugar deste marcador.
- ↑ Bek-Thomson, M.; et al. (2008). "Acne is Not Associated with Yet-Uncultured Bacteria". Journal of Clinical Microbiology 46 (10): 3355–3360. PMC 2566126. PMID 18716234. doi:10.1128/JCM.00799-08.
- ↑ Francois P and Schrenzel J (2008). "Rapid Diagnosis and Typing of Staphylococcus aureus". Staphylococcus: Molecular Genetics. Caister Academic Press. ISBN 978-1-904455-29-5.
- ↑ Mackay IM (editor). (2007). Real-Time PCR in Microbiology: From Diagnosis to Characterization. Caister Academic Press. ISBN 978-1-904455-18-9 .
